Navigating Your First Podiatrist Appointment: Tips to Ease Anxiety and Prepare for Success

Are you gearing up for your first visit to a podiatrist? Whether it’s due to foot pain, a concern about your gait (the way you walk), or a routine check-up, it’s normal to feel a bit anxious about seeing a new practitioner. Podiatrists are experts in diagnosing and treating conditions of the feet and lower legs, but stepping into a new healthcare setting can be daunting. Here’s how you can tackle your fears and ensure a smooth and successful appointment.

Understanding Your Podiatrist Appointment
A Podiatrist is a professional who specialises in the diagnosis and treatment of foot and ankle conditions. They can help with a variety of issues, from bunions and heel pain to sports injuries and diabetic foot care. Knowing what to expect can help reduce anxiety and make the experience more comfortable.
1. Learn About the Procedures
Before your appointment, familiarise yourself with common Podiatric procedures. Most visits will involve a thorough examination of your feet and ankles. The podiatrist might ask about your medical history, lifestyle, and any specific concerns you have. Understanding these basics can demystify the process and help you feel more in control.
2. Prepare Your Medical History
Having a detailed medical history on hand can streamline your visit. Include information about any current medications, past injuries, surgeries, or chronic conditions. If you have specific foot issues or pain, noting when they started and any activities that worsen them can be incredibly useful.
3. Dress Comfortably
Wear comfortable clothing and shoes that are easy to remove. Your Podiatrist will need to examine your feet and possibly ask you to walk, so choose attire that allows easy access to your lower limbs.

Overcoming Anxiety About Your Podiatrist Appointment
Feeling anxious about a new healthcare provider is common, but there are effective strategies to manage these feelings.
1. Ask Questions
Don’t hesitate to ask your Podiatrist about anything you’re unsure of. Whether it’s about the examination process, potential treatments, or follow-up care, having answers can ease your worries and help you feel more informed.
2. Bring a Support Person
If it helps to have someone with you for emotional support, bring a friend or family member to your appointment. They can offer comfort and assist with taking notes or asking questions.
3. Practice Relaxation Techniques
Before your appointment, try relaxation techniques such as deep breathing exercises or visualisation. These methods can calm your nerves and prepare you mentally for the visit.
4. Focus on the Benefits
Remember that seeing a Podiatrist is a step towards better foot health. Whether it’s alleviating pain, improving mobility, or addressing a specific concern, focusing on the positive outcomes can help shift your mindset from anxiety to anticipation.
Preparing for Your Podiatrist Appointment
Preparation is key to making the most of your visit and ensuring you get the care you need.
1. Compile Your Foot Health History
Make a note of any previous foot problems, treatments you’ve tried, and any noticeable changes in your feet or walking patterns. This information will help your Podiatrist understand your situation better.
2. List Your Concerns and Symptoms
Write down any symptoms you’re experiencing, such as pain, swelling, or numbness, and note when they occur. This will help you communicate your concerns clearly and allow the podiatrist to provide a more accurate diagnosis.
3. Bring Relevant Documentation
If you have any previous medical records related to your foot health or prior treatments, bring them along. This documentation can provide valuable insights into your condition.
4. Review Insurance and Payment Options
Check your insurance coverage and understand what is included for podiatric services. If you’re unsure about your coverage, contact your insurance provider before the appointment to avoid any surprises.

Final Thoughts
Visiting a new Podiatrist doesn’t have to be a stressful experience. By understanding what to expect, preparing thoroughly, and using strategies to manage anxiety, you can approach your appointment with confidence. Remember, your Podiatrist is there to help you achieve better foot health and improve your quality of life. With a bit of preparation and a positive mindset, you’ll be well on your way to a successful visit.
Embrace the opportunity to address your foot concerns and take a proactive step towards better health. Your feet—and your overall well-being—will thank you!
Contact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthy Feet: Essential Tips for Maintaining Optimal Foot Health


2. Preventing Common Foot Issues
a. Fungal Infections: To prevent athlete’s foot and other fungal infections, avoid walking barefoot in public areas like locker rooms or swimming pools. Wear moisture-wicking socks and change them daily. If you notice any signs of infection, such as itching or redness, consult with your Podiatrist for appropriate treatment.
b. Bunions and Hammertoes: Bunions and hammertoes can be uncomfortable and affect the way you walk. To prevent these conditions, wear shoes with a wide toe box and avoid high heels that put extra pressure on your toes. If you experience pain or notice any deformities, seek professional advice for management and treatment options.
c. Plantar Fasciitis: This common condition causes heel pain due to inflammation of the plantar fascia. To prevent plantar fasciitis, ensure you have proper arch support in your shoes and stretch your calves and feet regularly. If you experience persistent heel pain, consult a podiatrist for a tailored treatment plan.

3. Understanding Podiatric Conditions
a. Flat Feet: Flat feet occur when the arches of the feet collapse, leading to pain and discomfort. Symptoms can include aching feet, especially after standing or walking for long periods. Orthotic inserts and supportive footwear can help alleviate symptoms. In severe cases, surgical options may be considered.
b. Diabetic Foot Care: For individuals with diabetes, foot health is crucial to prevent complications such as ulcers and infections. Regularly inspect your feet for cuts, blisters, or changes in skin color. Maintain good blood sugar control and consult with a Podiatrist for specialised care.
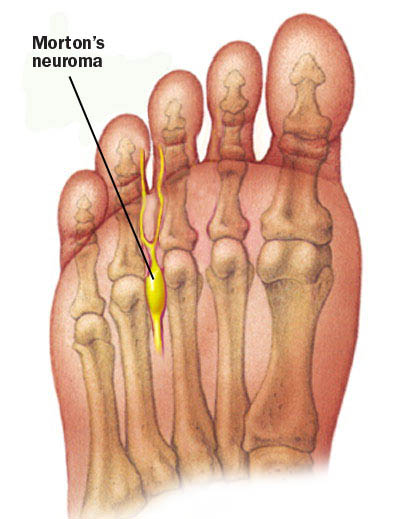
c. Morton’s Neuroma: This condition involves a thickening of the tissue around a nerve in the foot, usually between the toes. It can cause sharp, burning pain and numbness. Proper footwear, custom orthotics, and in some cases, injections or surgery, can help manage symptoms.
4. The Latest in Foot Health Research
Recent studies have highlighted the importance of foot health in overall well-being. Research shows that maintaining proper foot mechanics can significantly impact joint health and prevent chronic pain. Innovations in custom orthotics and advanced imaging techniques are improving diagnosis and treatment of foot conditions. Additionally, new insights into the relationship between foot health and systemic conditions like diabetes are leading to more comprehensive care strategies.
Conclusion
By incorporating these daily foot care tips and staying informed about common foot issues and conditions, you can take proactive steps towards maintaining healthy feet. Regular self-care and professional check-ups with a podiatrist will help you stay on top of your foot health and address any concerns before they become serious problems.
Contact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Fungal nail laser the best treatment for fungal toenails and onychomycosis?

Fungal nail laser the best treatment for fungal toenails and onychomycosis?
Nail fungus is an issue that has become more common in the 20th century, and it can be dangerous for your health in the long run. Nail problems like onychomycosis and nail fungus in general can end up severely damaging your toenails and that’s why you want to address the problem as quickly as possible. However, before we identify any onychomycosis treatment, it’s important to figure out what causes onychomycosis and fungal toenails and why such problems appear in the first place.
What is onychomycosis?
Onychomycosis is a common fungal infection that particularly targets your toenails. Generally, it affects the toenails, but the fingernails can also be affected sometimes. In addition, onychomycosis can also end up with complications like cellulitis for the lower leg. There are a variety of fungi that can lead to onychomycosis, like fusarium or dermatophytes.
A thing to note about onychomycosis is that it has certain risk factors that can worsen the situation. These include a bad immune function, peripheral vascular disease, exposure to someone that already has onychomycosis, but also various nail diseases, and athlete’s foot.
Nail fungus symptoms that you should know about
Usually, there are a few symptoms that appear before you have a nail fungus problem like onychomycosis. It’s very important to study your nails and see if they are discolored, thickened, ragged, crumbly, or brittle. Sometimes, nail fungus can end up making your nails distorted, and they might even be separated from the nail bed. Fungal issues can also make your nails or toes smelly, so that’s a thing to keep in mind.
Aside from that, you should consider talking with your doctor if you have difficulties walking due to your nails, if the area around your nails is bleeding, if you have diabetes and experience any of the symptoms above, or if you have any pain/swelling around the toenails. If that’s the case, then addressing such issues as quickly as possible becomes a major thing to focus on.
If you encounter these issues, you need to talk with a doctor right away. The problem is that if you just leave things untreated, the skin around and under your nails will be inflamed. It will be very painful to walk or move your fingers, which clearly becomes a problem in the long run. Aside from that, you can also end up with dermatophytids. These are skin lesions that are free of any fungus, but they do appear as an allergic reaction to that fungal problem.
What causes onychomycosis and fungal issues?
Mold, yeasts and dermatophytes can all lead to a fungal infection and problems like onychomycosis. Dermatophytes, in particular, are a major cause behind onychomycosis, especially if you live in western, temperate countries. Those people that live in the tropical and subtropical regions deal with humid, hot climates and that’s when candida tends to be the major problem behind fungal problems and onychomycosis in particular.
Aside from that, we should also note risk factors. As you get older and especially surpass 60 years old, you are more prone to fungal issues like onychomycosis. The reason here is that your blood circulation will not be as fast, and you will also have your nails grow slowly, not to mention they get thicker. The fact your immune system is not as effective as you get older also creates a perfect medium for onychomycosis as well.
But that’s not all; there are other risk factors, too. Wearing socks that hinder ventilation, having psoriasis, sweating a lot, going barefoot in damp places, having damaged nails, diabetes, or circulation problems can also be extremely problematic.
There are five different types of onychomycosis
- First, we have the distal subungual onychomycosis caused by the trichophyton rubrum. That invades the nail bed and it also goes under the nail plate.
- Candida onychomycosis is caused by candida, and it’s common among people who deal with a lot of humidity.
- Endonyx onychomycosis is generated by leukonychia.
- Proximal subungual onychomycosis happens when the fungus penetrates the nail plate via the proximal nail fold.
- Lastly we have the white superficial onychomycosis that tends to be caused by a fungal invasion.
Regardless of what kind of onychomycosis you might have, it’s imperative to ensure that you find the right treatment, and fungal nail laser can be the right option to consider in a situation like this!
How do you diagnose onychomycosis?
Diagnosis relies on 4 different approaches. You have the potassium hydroxide smear that can help identify onychomycosis cases and fungal infections with ease. A histology examination can help, and the same thing is valid when it comes to a polymerase chain reaction. Nail plate biopsy combined with some acid Schiff stain can be reliable as well.

Why is the Fungal Nail LASER the best treatment for onychomycosis and nail fungus?
When you try to treat something like onychomycosis, you will usually try out antifungal medication. However, these treatments aren’t always very effective, and you will need to use them for quite some time. Some topical agents can be used to treat onychomycosis, more specifically, amorolfine, ciclopirox nail paint, and many others. Just like other nail fungus treatments, it can take months or up to a year to see any results.
As you can see, regular treatments can only do so much, and they will take a long time until you actively see results. That’s why going for the fungal nail laser treatment is a much better idea. According to various studies, using fungal nail lasers can be extremely helpful and you get to see results a lot quicker. You can also use it in combination with topical anti-fungals since that can help increase its efficiency while also lowering healing time. The first step would be to book in for a fungus consult.
No anesthesia is needed!
Maybe the best thing about fungal nail laser treatments is that no laser is needed. The dermatologist will prepare the nail, and then the laser is pulsed using various wavelengths. Doing that helps lower any heat exposure to your skin, and there are little to no side effects because of that. Bleeding or a bit of pain tends to be normal, but you should talk with the dermatologist and ensure that there are no problems.
The recovery time is not very long
That’s the great thing about laser treatments for the toenail fungus. The doctor will give you instructions on how to keep the toe dry and clean. Depending on the situation, you might also receive some topical antifungal cream that you need to apply to the nail. It can take a few days until the fungus gets removed, and generally, you will have to go through multiple sessions.
What you can expect after a successful fungal nail laser treatment:
- Your nail will start growing again, and it will have a normal texture and shape.
- You will see that the nail will not detach from the nail bed as much, and that’s a sign of healing!
- There’s no flaky debris on or under the nail.
- You won’t have to deal with any brown, white, or yellow discoloration of your toenails.
As you can see, a fungal nail laser treatment is the ideal option if you want to deal with onychomycosis or any nail fungus efficiently. It’s not only a reliable, safe, and comprehensive treatment, but it can help you alleviate the pain caused by nail fungus problems such as onychomycosis. Combined with topical, antifungal cream, it can fully protect your nail and encourage recovery. That’s why the fungal nail laser comes as the best, highly recommended treatment for anyone who has onychomycosis! BOOK NOW.
Dr. Fatima Al-Kathmi (Podiatrist)
BOOK YOUR FUNGUS CONSULT NOWContact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Shockwave is an effective treatment for pain and injury. The purpose of the therapy is to trigger the body’s own natural healing response. Many people report that their pain is reduced and mobility improved after the first treatment. Is it for me? Book an initial biomechanics assessment to find out whether this is an appropriate treatment for you.
BOOK NOWShockwave Therapy for Heel Pain
If you’re dealing with heel pain or plantar fasciitis, then it’s very difficult to walk and perform your daily tasks. In fact, even the simplest tasks that require movement will be associated with excruciating pain, and that will limit your capabilities and things you can do. That’s where shockwave therapy for heel pain can be a very good idea.
What shockwave therapy does is it relies on soundwaves in order to stimulate healing. It’s particularly good for Achilles tendinopathy, plantar fasciitis or any similar type of heel pain. Soundwaves will help improve the bloodflow, and that can enhance, but also speed up the healing process as a whole.
How does shockwave therapy for heel pain work?
- – The entire process is very simple. A dedicated machine is used in order to apply soundwaves to the skin’s surface.
- – That machine’s probe is used to target a certain area, usually the area that causes a lot of pain.
- – Once the sound waves are generated, they will spread into the tissue and go outwards. What happens is the soundwaves increase the bloodflow. Your body will speed up the healing process, and you will also feel a lot better.
The advantage of going for shockwave therapy is that it will end up removing a lot of the pain that you are currently facing. Not only that, but it encourages your body to heal a lot faster. And, according to research, it’s very efficient. You can see progressive improvements, without dealing with any major side effects. That encourages everyone to not only give shockwave therapy a try, but also stick with it for more than one treatment.
Who is shockwave therapy for?
Most of the time, everyone dealing with heel pain should consider trying shockwave therapy. However, this therapy is particularly good for people that didn’t respond well to other treatments. If you tried ice therapy, steroid injections, orthotics or physiotherapy and none of them worked, shockwave therapy might be the answer.
That’s because shockwave therapy is offering you immediate relief. On top of that, it will help alleviate the pain for quite a long time. And it also helps your body recover and repair its tissues at the same time. It’s still important to talk with your doctor beforehand. The doctor will let you know if your current health status allows the use of shockwave therapy, or if there are any other treatments to try out.
Is there anything you can do to prepare for shockwave therapy?
If the doctor cleared you for shockwave therapy, then there are a few things you can do to prepare for it. Ideally, you don’t want to take any NSAIDs (non-steroidal anti-inflammatory drugs) around 2 weeks before the procedure. It’s important to check any medication you are currently taking and see if it has any NSAIDs. Also, you can wear comfortable clothing, there’s no need for any specific clothing pieces in order to undertake the shockwave therapy treatment.
Is shockwave therapy painful?
It always depends on how bad your current heel pain really is and what causes it. For the most part, you might experience some pain during the shockwave therapy procedure, that’s normal and something you will encounter. Thankfully, the shockwave power can be adjusted depending on how much pain you feel. That way, it’s not going to hurt as bad and you will still be ok. In severe cases, a local anesthetic might be necessary, but for the most part it won’t hurt that much or at all.
When you think about shockwave therapy, the first thing that comes to mind is that your body automatically reacts to it. Yes, you will feel your body responding to this extremely fast. What happens is your body will break down any calcifications find in your foot, boost the cell permeability and that can help with the healing process.
Another thing that shockwave therapy does is it encourages your body to create new blood vessels. That brings more nutrition and blood to the inflamed area. And, of course, the body will automatically target the nerve endings and hyperstimulate them, which means you will be feeling less pain.
Is shockwave therapy an invasive procedure?
No, shockwave therapy is designed to be a very safe and non-invasive procedure. In fact, what it does is it allows you to alleviate heel pain, while also making it easy to feel better. According to this study, shockwave therapy has a great chance of success, with up to 80% feeling positive results from the therapy process.
That’s also doubled down by another study which clearly shows how much it can help against muscle pain in particular. Even if you choose shockwave therapy, it’s still a good idea to make some lifestyle changes. Avoiding any activities that cause foot pain is mandatory, and you also want to use walking boots or crutches, as needed. Even simple changes like these can help reduce pain, and they will speed up the healing process!
What are the pros and cons for shockwave therapy?
Like any other therapy, shockwave therapy also has its own pros and cons. It’s important to talk with a medical professional and perform your due diligence if possible. That will make it easy to understand how to tackle heel pain efficiently, while also understanding if this treatment is suitable for you or not.
Pros
- – One of the best things about shockwave therapy is that, in most cases, it will provide immediate relief. That relief can end up lasting for a long time.
- – There’s no need for a very complex, long preparation process. The same thing is valid when it comes to recovery, you just need to take a few hours off and let your body heal.
- – It’s a procedure that has been tested for a long time, and studies show it’s safe.
- – The chances of dealing with complications are very low.
- – You don’t have to deal with surgery, since it’s a non-invasive procedure.
Cons
- – While it works for a lot of people, it won’t be for everyone.
- – In some cases, it might take multiple sessions until you see results.
- – There are some minor complications, like numbness, bruising or temporary pain.
- – It’s not covered by insurance companies, although that might depend on the situation.
How much does shockwave therapy cost?
The price of shockwave therapy will vary from one practitioner to another. It also depends on whether you are just getting the regular therapy, or you combine it with another package. But on average, the full course of shockwave over the 5-7 week period will end up costing you between $500 to $700, either more or less depending on the practitioner.
The exact cost will vary based on your location, how many sessions you need, if your insurance company will cover these costs, but also the intensity of the treatment. It’s a good idea to talk with a practitioner beforehand and ask for a quote. Not only will that help you save time, but you can also narrow down the ideal treatment that fits your needs.
Conclusion
As you can see, shockwave therapy for heel pain can be extremely efficient, and it’s not very painful either. In fact, it’s one of the best methods that you can use to alleviate your current heel pain. It’s very dependable, but you should talk with a medical professional first. Our team at The Foot Force Podiatry is here to deliver state of the art shockwave therapy solutions at amazing prices. Don’t hesitate and book an appointment with us today, we’ll help alleviate your heel pain in no time! Book an initial biomechanics assessment to find out whether this is an appropriate treatment for you.
Dr. Fatima Al-Kathmi (Podiatrist)
Contact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Chronic Venous Insufficiency

Introduction to Chronic Venous Insufficiency
Your arteries are pipes inside your body that carry blood from your heart to the rest of your body and your veins carry blood back to your heart from the rest of your body. Veins have one-way valves that prevent the blood from flowing backward, to ensure they reach your heart properly.
When your vein walls and valves are damaged, the veins cannot manage blood flow as well as they should and it is harder for blood in your legs to return to your heart. This causes a pool of blood in your legs and increases the pressure on the walls of the veins; this is known as chronic venous insufficiency.
Chronic venous insufficiency is most commonly caused by blood clots (deep vein thrombosis) and varicose veins. In some cases, weakened leg muscles have trouble squeezing blood upwards and can contribute to venous insufficiency.
Other risk factors include obesity, pregnancy, sitting or standing for long periods of time without moving, and family history of venous insufficiency.

What are the symptoms of venous insufficiency
- Swelling of the leg and ankle
- Itchiness of the legs
- Aching, throbbing, or heaviness of the legs
- Leg ulcers
- Pain that gets worse when you’re standing and gets better when you raise your legs (worse at night when sleeping)
- Skin changes especially around the ankle

How to treat venous insufficiency
Without treatment, the pressure and swelling will burst the tiny blood vessels in your legs called capillaries. This can result in skin changes such as reddish brown discolouration especially near the ankles which can lead to swelling and ulcers. The below are some ways to treat and improve venous insufficiency at home:
- Wear compression stockings to help with your blood flow return and relieve symptoms
- Lifestyle changed such as exercise and diet to improve your blood flow
- Stop smoking to improve your blood flow
- Calf muscle movement while sitting or standing for long periods of time
- Maintain good skin care by moisturising daily
- Elevating calves when laying down or sitting down
- Calf raises to activate the muscle pump that helps the blood flow up to the heart
The above measures may not be sufficient in treating your condition, and seeking medical advise from your Doctor is the best way to treat and look after your venous insufficiency. It is also advisable to speak to your Podiatrist about your concerns.
The Foot Force Podiatry
Contact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Ankle Instability
and Pain

Ankle instability or ‘weak ankles’ is very common, especially when there has been a previous injury, such a sprain to the ankle. Weak ankles can affect balance and increase your risk of sprains which can lead to chronic ankle instability. Weak ankles can sometimes be caused by genetics, ligament laxity or even inappropriate footwear.
Chronic ankle instability is a condition characterized by ‘giving way’ of the outer side of the ankle. This condition often develops after repeated ankle sprains. Many athletes, as well as non-athletes, suffer from chronic ankle instability.
40% of people who suffer their FIRST ankle sprain will go on to suffer from chronic ankle instability within the first year since it has occurred. Inappropriate or inadequate ankle rehabilitation following an ankle sprain may result in chronic ankle instability.
There are many reasons why someone may have weak ankles. However, there are many things we can do to fix it!

What are the signs and symptoms of ankle instability?
- Repeated turning of the ankle, especially on uneven surfaces or when participating in sports
- Persistent discomfort and swelling
- Ankle pain or tenderness
- Ankle feeling wobbly or unstable (poor balance)

Treatment:
- RICER: Rest, Ice, Compression, Elevation, Referral (to see a Podiatrist)
- Medications: Non-steroidal anti-inflammatory medication to help alleviate the pain and inflammation (temporarily)
- Bracing: provide appropriate support to your ankle and prevent your ankle from turning. It also allows the injured area to heal properly while allowing you to remain mobile
- Ankle rehabilitation: to strengthen the ankle, improve balance and range of motion, and retrain your muscles – See a Podiatrist for efficient rehabilitation
- Foot mobilisation: to restore normal function of your joints and bones of the foot and ankle – See a Podiatrist for efficient ankle mobilisation treatment

Preventative Measures:
- Stretching exercises prior to commencing exercises
- Wear appropriate footwear; avoid high heels
- Be extra careful when doing exercises on uneven surfaces
- Do ankle strengthening exercises
- Seek a Podiatrist for more personalised advice and treatment
Here at the Foot Force Podiatry, we offer a range of treatment options to help with rehabilitation and prevention of ankle instability. Book your initial biomechanical assessment NOW!
Book OnlineContact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Best thongs with arch support recommended for foot pain

Best arch support thongs for foot pain?
If you suffer from heel pain, foot pain, knee or calf issues, you’ll know all too well how debilitating poor foot support can be. Unfortunately, many common brands of thongs do not accommodate to users with regular foot pain and associated conditions.
When the time comes to select new footwear, your best pathway is to opt for thongs for foot pain that are directly endorsed by podiatrists and physiotherapists. Arch support footwear is also a great alternative for those without existing foot pain and conditions.

The Importance of Arch Support
Feet are not all the same. On the whole, there are three main arch variations – a normal arch, a flat arch or a high arch. As a result, the level of tailored foot support required will vary from individual to individual.
Proper arch support can have a major impact on your day-to-day life. Arch support is particularly crucial for foot alignment and the reduction of pain or swelling. If your doctor has recommended thongs for foot pain, it is vital that you look for styles that specifically accommodate to your distinct arch support requirements.

No Compromise on Style
You no longer have to rely on flimsy rubber soles. Over recent years, the orthopaedic footwear industry has taken a number of significant strides. Purpose designed thongs for foot pain not only serve their primary function, but also bring first-class style and comfort.
Numerous men’s and women’s styles now exist that resemble traditional looks, yet feature the added benefits of certified arch support. In addition, the wealth of choices on offer means that you are no longer confined to one or two variations.

Contoured Footbeds
For extra cushioning and support, you can never go wrong with a contoured footbed. A contoured footbed is an inbuilt curved liner that directly cushions the heel and toes. Many new thongs for foot pain will feature this technology and therefore provide excellent daily support.
Any contoured footbed should match the individual shape and natural arch of your foot. This factor will ultimately influence the thongs that you select. Contoured technology is also excellent for maintaining consistent stability as you walk.

A Few of the Best
To make your choice a little easier, we have compiled a list of the best podiatrist certified thongs on the market. Read on below for dynamic compilation of men’s and women’s styles.
Women’s Zullaz Range
The women’s Zullaz collection of orthotic thongs features a number of stylish alternatives. Of course, each individual option comes with purpose built qualities well suited to foot pain sufferers. Zullaz flip flops are excellent for foot pain, offering five star treatment on each and every use. You can not only find a tailored option, but also various colours to match your personal preference and style.
Men’s Zullaz Range
The Zullaz range isn’t exclusive to women. For all the men out there with regular foot and leg pain, they too can access 5 star treatment. Fitted with excellent arch support, comfortable materials and contoured footbeds, Zullaz represents the latest in podiatrist recommended technology. Similar to the women’s range, men’s Zullaz footwear is also offered in a diverse set of styles, colours and fabrics. The choice will be all yours.

Archies Support Thongs:
The Archies support thongs features aim to support the foot in a more biomechanically appropriate position. This means that the stresses and strains that are put on the foot structures are reduced. They have up to 2.2cm of orthotic support and incorporate the same amount of support that you would find from a prefabricated or off the shelf orthotic. Archies have aimed to make their support thongs look as much like normal thongs as possible without compromising on the support for the feet. The Archies support thongs are very comfortable, and made from high quality foam material. Once you get used to them, you will not want to wear any other thongs. They have many colours to choose from.

Birkenstock EVA Flip-Flops
In the world of footwear, Birkenstock is synonymous with style and comfort. Their EVA flip flops for foot pain are no different. With contoured technology and flexible insoles, these sandals can be adjusted to the unique shape of your foot. During use, they will also cradle each and every curve across your arches.
Another key feature of these thongs are the cork base/footbed. This base naturally absorbs shock to support everyday movement and ensure comfort at all times.

Clarks Breeze Sea Flip-Flops
If you prefer a lightweight feel, the Clarks Sea Breeze series will provide everything that you need. Once purchased, you can slide them on and experience the superior grip of a synthetic rubber sole base. Other first-class features include the OrthoLite footbed and ultra-soft textile lining.
Within the market of thongs for foot pain, the Sea Breeze series is perfect for those with sensitive feet and require a nice and soft underfoot feeling.

Olukai Ohana Flip-Flops
Foot pain can arise at anytime. When the summer hits, foot pain sufferers should still be able to enjoy the beach in style and comfort. This is where Olukai Ohana thongs fill the void perfectly. With water resistance and quick-dry technology included, this supportive footwear allows you to enjoy the outdoors and take your mind off foot pain.
Like the men’s and women’s Zullaz range, Olukai Ohana flip flops come in a wide array of fresh and vibrant summer colours. Don’t bring foot pain with you on your next vacation, opt for premium podiatrist footwear instead.

Reef Ortho-Bounce Woven Flip-Flops
Reef are a premier Australian brand that specialise in outdoor footwear. In the realm of thongs for foot pain, Reef’s ortho-bounce series are a one of one – a rare combination of function, style and comfort. The woven strap upper is also made from recycled material with vegan leather detailing, making this an excellent ecofriendly option.
Similar to Birkenstock’s ortho sandals, Reef’s woven flip flops are shock absorbent and aid you with each step. The rubber outsole is also fitted with rubber flex grooves that provide extra traction and durability, ensuring that your receive value for money.

Contact a Professional for Assistance
For a comfortable and fashionable orthotic option, it’s hard to look past leather sandals and thongs. Some of the best leather podiatrist-recommended thongs providers include Archies, Aerothotic, Zullaz, Olukai, Rainbow, Reef and more.
In this context, professional assistance could come from a Podiatrist. Once a recommendation is made, you can then browse all the orthotic thongs on the market and make a purchase that suits your individual needs. Any of the aforementioned options are high-quality and the product of innovative medical design.
Nivi Watson
Experience Guest Blogger
Contact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Plantar Plate (Ball of Foot) Pain
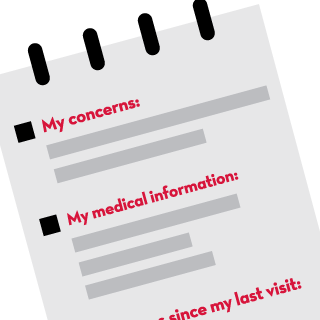
Ball of Foot Pain
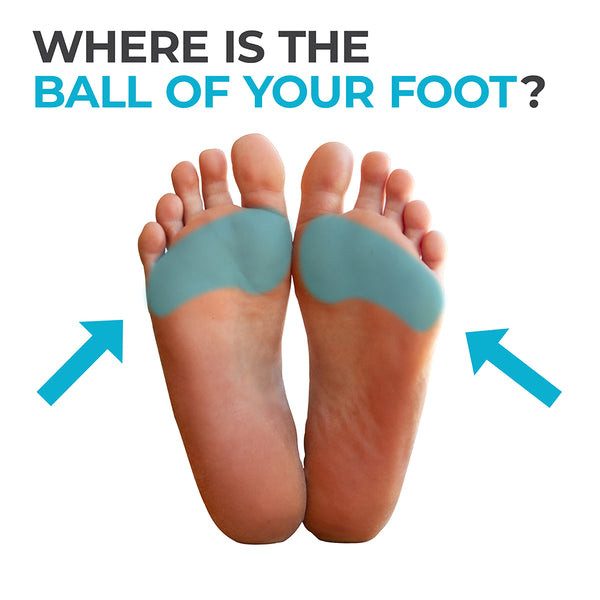
Pain that is felt in the ball of the foot (the area just before the toes as shown on the image on the left) is quite common among the general public and can be caused by a number of reasons. In most occasions, people who are experiencing the pain in this area are labelled as having ‘metatarsalgia’ which is a very vague and common term used to explain pain in the ball of the foot. People with ball of foot pain tend to feel an aching pain and inflammation in this region. Some may even feel a sharp shooting pain, numbness, and even pain when flexing the toes.
As a Podiatrist that deals with many biomechanical cases with my patients, it is the second most common concern I hear and see in the clinic. There are many causes and reasons as to why people get pain in that area of the foot, and one of the most common culprits is ill fitting shoes! In most cases, the types of shoes that increase the risk of pain in the ball of the foot are shoes with a heel. The reason for this being is that, normally, this is the area where people place most of their weight when standing and walking. Wearing a shoe with a heel will increase the pressure and load on the ball of the foot, causing issues and pain.

The Symptoms of Pain in the Ball of Foot
Some symptoms that may be experiences when having issues in this region, may include, but is not limited to:
- Aching or burning type of pain in the front of the foot.
- Sharp, shooting pain which can run the length of any of the toes, be generalised to the front of the foot, or can be specific to one spot.
- Numbness, tingling or a pins and needle sensation in the toes.
- Feeling like there is a small pebble inside of your shoe.
- Immediate pain which gets worse when standing, walking, running, exercise or flex your foot and toes.
Ball of foot pain can also occur simultaneously with inflammation, swelling, or bruising of the foot.
What are the risk factors for ball of foot pain?
The risk factors that can be leading to pain in the ball of the foot are:
- Having a high arched foot causes an increase pressure at the ball of the foot.
- Having the second toe longer than the first: this can cause an increase pressure at the base of the joint, where it connects at the ball of the foot.
- Being overweight which can lead to an increase in pressure and weight on your feet.
- Intense physical activity which can lead to increased pressures on the ball of the foot.
- Wearing heeled shoes (even a small heel) or shoes that are too tight can increase pressures on that region of the foot.
- Having toe deformities can lead to increased pressures on the feet.
- Age: The fatty pad that provides cushioning to that region of the foot diminishes with age, increasing pressures on ball of foot. Arthritis usually increases with age, which can cause damage and increased pressures on the ball of the foot.
What Conditions can be causing Pain in the Ball of the Foot?
If left untreated, it can affect the way you walk and cause more complex conditions which may take longer to treat. The conditions that can be causing pain in the ball of the foot are:
- Plantar plate tear: A very common injury which is caused by repetitive overload of the ligament (plantar plate) located at the bottom of the toe and attaches to the ball of the foot. It is most commonly seen in the second toes.
- Capsulitis: inflammation of the surrounding structures of the joints in the region of the ball of foot.
- Morton’s neuroma: Thickening of the tissue around a nerve running the length of the toes. It is most commonly felt between the 3rd and 4th toes.
- Sesamoiditis: The structures around the little bones at the big toe joint become inflamed due to overload.
- Stress fracture: Repetitive load on the ball of foot can lead to a stress fracture of the metatarsals (bones that connect the ball of foot to the toes)
- Corns and/or calluses: Increase loads and pressures on the ball of the foot which can be caused from poor fitting shoes or a high arched foot can lead to hardening of the skin in that region. The hardening of the skin is called callus or corns.

How can I Treat my Ball of Foot Pain at Home?
The following changes can be made at home to relieve some of the pain and pressure that you are getting on the ball of the foot:
- Footwear: Wear shoes that are wide enough to allow movement at the toes when walking and when you are on your feet. Ensure the shoe you are wearing does not have a heel to reduce the pressures on the front of the foot. Please follow our guide to choose a good shoe for your foot by clicking here.
- Rest your foot when you can, especially after activity. Placing your feet in an ice water bath for 2o minutes every 4 hours may help relieve any pain, inflammation and swelling.
- Stretching: Where activity may be causing you pain, targeted stretching can help ease the pain, increase flexibility and improve strength. Ensure you do stretches a few times a day until you feel the pain has reduced.
- Manage Body Weight: Excess body weight can increase the load and pressures put not the ball of the foot. Reducing weight will relieve the loads on the joints and feet. We recommend seeing your GP to help you with weight loss and management.
- Pain medication: taking ibuprofen or Panadol as directed by your Doctor help alleviate some of the pain. Please keep in mind that pain killers only mask the pain and do not treat the cause, meaning that the pain will come back.
If you have tried the above mentioned home care advice for ball of foot pain and have no relief after 1 month, it is safe to say that the pain will not go away on its own. It is time to see a Podiatrist for an initial biomechanical assessment to figure out why you are experiencing pain and how we can help to alleviate it. Your Podiatrist will give you a tailored treatment plan which may include footwear change based on your foot type, stretching and strengthening rehab exercises and possibly:
- Custom Orthotics: Depending on the severity of pain, and also the condition that is causing your pain, your Podiatrist might prescribe you custom orthoses which will help treat the pain at the cause, relieve the pain you are experiencing and also reduce the ris of the pain returning in the future.
- Shockwave Therapy: Depending on your condition and why you are experiencing pain, your Podiatrist might recommend shockwave therapy to help heal your condition and relieve pain.
Dr. Fatima Al-Kathmi (Podiatrist)
The Foot Force Podiatry
BOOK NOWContact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Winter Chilblains

What is Chilblains?
Chilblains is the inflammation of the little blood vessels in your skin as a response to repetitive cold weather exposure. It is often painful and more commonly seen on the extremities such as the toes, fingers and nose.
It is a misconception that the weather needs to be freezing before you see symptoms of Chilblains. It can be seasonal and occur more often in the colder months of the year. You can get Chilblains from repetitive cold (not freezing) weather exposure.

What causes Chilblains?
The cause of Chilblains is still unknown. There are some theories that it is the body’s reaction in response to cold weather exposure, followed by rewarming. In some cases, rewarming cold skin can lead to the abnormally rapid expansion of smaller blood vessels under the skin, leaving this trauma response (Chilblains).

What are the risk factors for Chilblains?
The factors that may increase the risk of having Chilblains or it’s symptoms may include:
- Gender: women are more likely to have Chilblains compared to men
- Underweight: If you weight 20% less than your normal BMI, you have an increased risk.
- Poor circulation: If you have less than normal blood flow, your body is more sensitive to changes in temperature, making you more likely to get Chilblains. e.g. smoking.
- Clothing: If you tend to wear tight clothes and shoes in cold and damp weather can increase your risk of Chilblains. Same goes for wearing clothing that exposes your skin to cold, damp weather conditions.
- Environment and Season: Chilblains are less likely to occur in areas where the weather is colder and drier as people in those areas are more likely to wear warmer clothing. There is more of a risk of Chilblains when living in a humid and colder (but not freezing) area. Chilblains are more commonly seen in colder months.
- Raynaud’s Disease: Increases the risk of Chilblains.
- Autoimmune Disorders: Lupus is the most common autoimmune condition to increase the risk of Chilblains.
- Occupation: Working in colder environments such as delivering freezable goods, having to enter freezer rooms and other similar professions tend to have an increased risk of Chilblains.

What are the symptoms of Chilblains?
Some symptoms for Chilblains may include, but is not limited to:
- Changes to skin colour (red/brown, dark blue, or purple)
- Pain at areas where the skin has changed colour
- Blistering or skin ulcers
- Itchy red patches on the skin of your hand or feet
- Burning feeling
- Swelling of your skin (especially toes or fingers)

How do I treat Chilblains?
Unfortunately, there is no cure for Chilblains. However, it usually clears up between one to three week’ time. This is also the case as the weather gets warmer. The best approach is to limit the exposure to the cold. Some things you can do to help ease and prevent the symptoms includes:
- Using certain lotions to ease the symptoms (please consult with your GP or Podiatrist before hand)
- Protecting yourself from the cold by wearing: a beanie, gloves and thermal socks (especially in the colder months)
- Limit your expose to cold weather or environments
- Cover all exposed skin as completely as possible when going out in cold weather
- Keep your skin, hands, feet and face dry and warm
- Keep your home and workplace warm
- Quit smoking
Chilblains do not usually cause permanent damage or injury. However, it can lead to infection, and if left untreated can cause damage.

Precautions and Complications of Chilblains:
If you have Chilblains and do not manage appropriately, you can get complications if your skin blisters and ulcers. Other than being very painful, it can lead to serious life-threatening infections if left untreated. Please see a Doctor if you suspect any infection (red, hot, swollen, pus).
It is important to keep any exposed skin as warm as possible. If you have Chilblains it is very important to GRADUALLY warm up your skin. Most people who are experiencing Chilblain symptoms have reduced sensation to heat or pain stimuli. DO NOT do the following things to warm up:
- DO NOT have a hot bath or shower.
- DO NOT place your feet or hands near a heater or hot water bottle.
- DO NOT use a hair dryer to warm up your hands, feet or face.
- DO NOT use an electrical heat blanket or doona.
Dr. Fatima Al-Kathmi (Podiatrist)
The Foot Force Podiatry.
Contact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Chronic Venous Insufficiency

What is an ingrown toenail?
An ingrown toenail is a toenail which has grown inwards into the skin, and often causes pain on the sides of the toe. This is commonly seen on the two big toes of each foot and may lead to infections which can leave the toe red, swollen, painful, and sometimes have pus coming out of it.
Ingrown toenails are very common, approximately 20% of people who visit their Doctor complain about ingrown toenails. In most occasions, these people are given antibiotics and asked to soak their feet in warm water with Epsom salts. However, the infection will persist if the offend nail is not removed.

WHAT CAUSES INGROWN TOENAILS?
- Poor toenail cutting technique – The nails should be cut straight across the top when cutting your nails at home. Cutting your nails too short, or cutting the sides of the toenails yourself can increase the risk of having ingrown toenails. This is because you may leave behind a spicule which can grown out into the skin and cause complications.
- Trauma to the toenail and surrounding skin – Pulling, ripping or cutting down the sides of the nail yourself increases the risk of getting ingrown toenails. It is best to have the ingrown toenail and surrounding skin by your Podiatrist to reduce the risk of complications in the future.
- Poorly fitted footwear – Wearing shoes that are too tight or that may not have enough room for your toes can lead to pressure on the skin surrounding the nail and cause them to curl inwards, and this can lead to ingrown toenails. Sometimes the curling of the toenail into the skin is permanent and cannot be fixed, unless you have surgery to remove that side of the nail permanently.

WHAT ARE THE RISK FACTORS FOR HAVING INGROWN TOENAILS?
- Genetics – As frustrating as it is, ingrown toenails can be genetic. Your mum, dad, uncle, aunty or even a second cousin may have ingrown toenails. You would of received the same genes that predisposes you to ingrown toenails.
- Adolescents – During this period of life, the feet tend to perspire more, meaning the nail and skin soften, which may lead to ingrown toenails.
- Reduced ability to care for nails – Not taking care of your nails, or trying to take care of them when you physically cannot reach them can cause trauma and increase the risk of having ingrown toenails.
- Poor nail habits – Cutting the nails too short or trying to round the corners can encourage the nails to grown into the skin.
- Sports – Participating in activities that involve running or kicking, such as soccer, can increase the risk of trauma and injury to your toes. This leads to ingrown toenails.
- Health Conditions – Conditions that poor blood flow, such as Diabetes can increase the risk of ingrown toenails.

HOW CAN I PREVENT INGROWN TOENAILS AT HOME?
To help prevent the risk of ingrown toenails:
- Correct cutting technique – Ensure you only cut your nails across the top. Any removal of an ingrown toenail should be removed by your Podiatrist.
- Maintain moderate length nails – Ensure you maintain a healthy length of nail by NOTcutting your toenails too short. If the nails are cut too short, pressure from your shoes can encourage the nails to grown into the skin around the nail.
- Wearing proper fitted footwear – Ensure your shoes are the right size and not too small. It is also important that you DO NOT wear shoes that are too tight or are ‘pointy’ from the front. If you have nerve damage (neuropathy) in the feet, you may not be able to feel wether your shoes are too small or tight.
- Wearing protective footwear – If you engage in activity that increases your risk of injury or trauma to your toes, you will need to wear protective (steel-cap) boots or shoes to protect your feet from injury.
- Check your feet regularly – It is important to check your feet daily for any signs of ingrown toenails or other foot problems (red, hot, swollen, pus, pain).
- Seeing a Podiatrist – If you are unable to do your own toenails due to health complications or age, you may be eligible for a GP Care Plan which means you will be eligible for up to 5 medicare rebated visits per year. At the Foot Force Podiatry, we bulk-bill general treatments to maintain your skin and nail care. All you need to do is see your GP and ask wether you are eligible.

WHAT TREATMENT IS AVAILABLE FOR INGROWN TOENAILS?
When seeing a Podiatrist for ingrown toenails, your treatment is dependant on the severity, wether you have risk factors and/or the reason(s) that you get them. If this is the first time you experience an ingrown toenail and you think it may be caused from wearing tight shoes, conservative treatment will suffice.
Conservative treatment consists of a general treatment where the offending nail edge will be removed. In cases where the ingrown toenail is very painful, local anaesthetic can be given to numb the toe for a painless experience. This will give an opportunity for the toe and skin around the nail to heal. It will also reduce a lot of the pressure and reduce the pain dramatically.
In cases where the ingrown toenail is always coming back, and is causing issues on a regular basis, it is more appropriate to have nail surgery to remove the ingrown toenail long-term. At our clinic, we have seen up to 99% success rate with ingrown toenail surgery.

What is ingrown toenail surgery?
Ingrown toenail surgery, also known as a partial nail avulsion (PNA) is a surgery which provides a permanent solution to your ingrown toenail. It is commonly done on the big toes, but can also be done on the little toes. Usually, only a small portion of the nail needs to be removed, not the whole nail.
The Podiatrist will first numb the toe with an injection to ensure the surgery is pain free. A tourniquet is applies around the toe (see the green band around the big toe on the image on the right) to stop any bleeding. The Podiatrist will then seperate the nail from the skin and remove only the part of the nail that is causing problems. Once that part of the nail, the nail root and any dead skin is removed, the Podiatrist will use a chemical called phenol to kill the nail root inside the toe to make sure that side of the nail does not grow back anymore. Your toe will be bandaged and some home care instructions will be given to you. You will need to come back to see your Podiatrist in 2-3 days for a check up and redress.
If you feel like you would benefit from the surgery, please book in for a ‘pre-surgery consultation and assessment for ingrown toenails’ with our expert Podiatrist.
Dr. Fatima Al-Kathmi (Podiatrist)
The Foot Force Podiatry.
BOOK NOWContact Us
Send us an e-mail:
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.